Peripheral vein disease
 2021-11-25
2021-11-25 Peripheral venous disease refers to a syndrome characterized by a series of symptoms and signs caused by abnormal venous structure or function, and excessive venous pressure, such as heaviness of lower limbs, fatigue and pain, edema, varicose veins, skin nutrition Changes and venous ulcers are the main clinical manifestations. Peripheral veins refers to the general term for veins of medium size or below that are located outside the chest and abdominal cavity. It refers to the veins of the head, neck and extremities, mainly including the internal jugular vein and external jugular vein of the head; the veins of the hands of the upper extremities, The veins of the arm include the cephalic vein, the median cubital vein, the axillary vein, and the subclavian vein. The veins of the lower extremities mainly include: the small saphenous vein, the great saphenous vein, the femoral vein and the communicating vein; the medial femoral circumflex vein, the lateral femoral circumflex vein and other veins.
Peripheral venous diseases account for about 60% of peripheral vascular diseases. Peripheral venous diseases mainly include varicose veins, deep vein thrombosis, and iliac vein compression syndrome. According to the data of Frost & Sullivan, the incidence of varicose veins in China is 10%-40%, the incidence of deep vein thrombosis of the lower extremities is 10%-20%, and the incidence of iliac vein compression syndrome is 20%- 34%. In 2019, there were 390 million patients with varicose veins in China; 1.5 million patients with deep vein thrombosis; and the incidence of iliac vein compression was 700,000.
The onset of peripheral venous disease is mild, the symptoms are not obvious, and it is easy to recur, causing the patient's condition to be easily delayed. The patient base is large, but many patients do not realize that the venous disease needs to be treated, and the best treatment period is missed during the treatment. Doctors sometimes lack treatment awareness. These comprehensive factors have led to insufficient attention to venous diseases. Venous diseases may cause complications such as pulmonary embolism and sudden heart disease in the later stages. Pulmonary embolism is the third leading cause of cardiovascular death after coronary heart disease and stroke, and is known as the "invisible killer."
Varicose veins is the most common venous disease. It is caused by blood stasis, weak venous wall and other factors, which lead to tortuous and dilated veins of the lower extremities. In the later stage, active ulcers and thrombosis may appear. Varicose veins are more common in women, mainly because estrogen affects the structure of the veins, or pregnancy increases the pressure on the veins of the pelvis and legs. According to statistics, about 70% of lower extremity varicose veins occur in the great saphenous vein, about 20% occur in the small saphenous vein, and about 10% of other types of varicose veins. Its onset is hidden and it is an "invisible killer" that cannot be ignored and may cause serious complications, such as fatal pulmonary embolism. High ligation and stripping of the great saphenous vein is a traditional surgical treatment, which is still commonly used today, but the surgical trauma is relatively large. Thermal ablation, foam sclerosant, emerging CHIVA (Conservative and Hemodynamic treatment of the Venous Insufficiency in an office based setting), and vascular closure belong to minimally invasive treatments. Radiofrequency ablation is the mainstream of thermal ablation therapy, which transfers energy to the vein wall in the form of heat energy, thereby occluding the diseased vein.
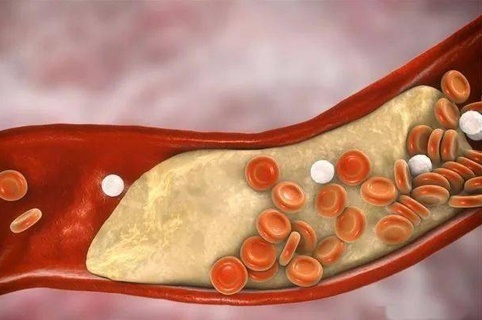
Deep vein thrombosis is a disorder of venous return caused by abnormal blood coagulation in deep veins. There are three main pathogenic factors-vascular wall damage, slow blood flow, and abnormal blood coagulation. Therefore, pregnant women and orthopedic surgery patients are more likely to Deep vein thrombosis appeared. In clinical practice, only a few patients with deep vein thrombosis have obvious symptoms, and the proportion of early missed diagnosis and misdiagnosis is relatively high. However, deep vein thrombosis may be life-threatening and cause complications including pulmonary embolism (PE) and post-thrombotic syndrome (PTS). 20%-50% of patients with deep vein thrombosis may suffer from post-thrombotic syndrome. The symptoms range from mild edema to pigmentation of the lower extremities, and severe patients even have venous ulcers. The disease is common in clinical practice and brings burden to patients. Heavy and expensive. Pulmonary embolism is the third leading cause of cardiovascular death after coronary heart disease and stroke, and deep vein thrombosis is collectively called venous thromboembolism (VTE). In pulmonary embolism, 75%-90% of the thrombus comes from the thrombus in the deep veins of the lower extremities and the pelvic venous plexus. In patients with deep vein thrombosis, pulmonary embolism occurs in nearly 50%. For deep vein thrombosis, in addition to the first choice of anticoagulation therapy, there are four interventional therapies—catheter contact thrombolysis (CDT), percutaneous mechanical thrombectomy (PMT), percutaneous transluminal angioplasty combined with stents Implantation, inferior vena cava filter placement. Catheter contact thrombolysis is the direct action of drugs on the thrombus through a catheter, and the new percutaneous mechanical thrombolysis in the third edition of the "Guidelines for the Diagnosis and Treatment of Deep Vein Thrombosis" , Shred, remove, dissolve or liquefy thrombus. Among them, the thrombus aspiration catheter can give negative pressure to directly suck the thrombus out of the blood vessel. For patients who have developed deep vein thrombosis and are at high risk of shedding, more and more recoverable or temporary vena cava filters are used clinically to prevent the occurrence of recurrent pulmonary embolism.
Iliac vein compression syndrome, also known as Cockett syndrome, refers to iliac vein compression from the anterior part of the iliac artery, leading to changes in lumen adhesion, lumen stenosis, or venous occlusion, resulting in iliac vein obstruction and a series of clinical trials. Symptomatic syndrome, the disease is mainly caused by the anatomical factors of the iliac vein. In 2019, the number of cases of iliac vein compression syndrome in China was 700,000, and the compound annual growth rate from 2019 to 2030 was 10.1%. It is estimated that the number of cases will reach 2 million by 2030. For patients with asymptomatic or mild symptoms of iliac vein compression syndrome, conservative treatment should be adopted, elastic stockings should be worn to improve living habits, avoid prolonged bed or sedentary sitting, and anticoagulant drugs can also be taken. For patients with lower limb venous thrombosis in the later stage, endovascular angioplasty can be performed, with balloons and stents implanted. With the continuous development of minimally invasive techniques, special venous stents have become the first choice for the treatment of iliac vein compression syndrome.